
Diabetes: Definition of the Disease
Glucose is a type of sugar and is the body's main source of energy.
Prevalence

Classification of diabetes
type 1 diabetes

Type II diabetes
other specific types of diabetes
gestational diabetes
causes of diabetes
- A malfunction in the immune system, causing it to attack pancreatic cells;
- Genetic disorders that impair tissue sensitivity to glucose, alter pancreatic function, and reduce or completely stop insulin synthesis required for glucose absorption;
- Viral infections: Coxsackie virus, rubella, Epstein-Barr virus, and retroviruses can penetrate pancreatic cells and destroy the organ;
- Chronic diseases affecting the pancreas, cystic fibrosis, pancreatitis, hemochromatosis;
- Endocrine diseases Cushing's syndrome, acromegaly;
- Toxins (e. g. , rodenticides used to kill rodents, heavy metals, nitrates);
- Dietary Habits Too much fat and simple carbohydrates in the diet can lead to obesity and reduced cell sensitivity to insulin;
- Medications, certain hormonal drugs (especially glucocorticoids), certain drugs to treat heart and nervous system conditions, B vitamin preparations (if taken in excess).
risk factors for diabetes
- Genetics – If you have a blood relative with diabetes, you are more likely to develop the disease;
- Some viral infections (eg, rubella, infectious mononucleosis) trigger an autoimmune response in the body, causing the immune system to attack pancreatic cells.

- overweight and obesity;
- Sedentary lifestyle (without physical activity, glucose is broken down more slowly, so cells may become less sensitive to insulin);
- A blood relative has diabetes;
- Aged over 45 years old;
- Prediabetes is a disease in which glucose levels in the blood remain at the upper limit of normal for a long period of time. Prediabetes is considered present if the analysis shows a value between 5. 6 and 6. 9 mmol/l;
- Having diabetes during pregnancy (gestational diabetes);
- Children weighing more than 4 kg at birth;
- frustrated;
- Cardiovascular diseases;
- Arterial hypertension (pressure above 140/90 mm Hg);
- High levels of "bad" HDC (more than 0. 9 mmol/L) and triglycerides (more than 2. 82 mmol/L);
- Polycystic Ovary Syndrome.
symptoms of diabetes
- intense thirst;
- weakness;
- Frequent urination;
- Bedwetting in children who have not previously wetted the bed;
- Sudden weight loss for no apparent reason;
- persistent and intense hunger;
- Frequent urinary tract infections or fungal infections.
- itchy skin;
- nausea;
- Vomit;
- stomach ache;
- dry mouth;
- muscle weakness;
- blurred vision;
- Poor wound healing;
- numbness in fingers or toes;
- Acanthosis nigricans darkens the skin of the neck, armpits, elbows, and knees;
- Diabetic skin disease is located in the bend of the lower limbs. Pigmented spots with skin atrophy and peeling often occur due to poor wound healing on the legs;
- Diabetic pemphigus causes blisters on the lower limbs, ranging in size from a few millimeters to several centimeters. Most commonly occurs in older patients with long-standing diabetes;
- Headache;
- The odor of acetone emanates from the mouth.

Diabetes complications
Continuously monitoring blood sugar and taking medications to lower blood sugar levels can prevent or delay the irreversible complications of diabetes.
diabetic coma
- The body is shaking,
- Chills,
- Dizziness,
- nervous or anxious
- severe hunger
- nausea,
- blurred vision,
- Heart rhythm disturbance.
In rare cases, low blood sugar may cause a person to pass out. In this case, he required an emergency injection of glucagon, which was administered by ambulance personnel.

- strong thirst
- Frequent urination,
- extreme fatigue
- blurred vision,
- Acetone or fruity breath smell,
- nausea and vomiting,
- stomach ache,
- Shortness of breath.
If such symptoms occur, you should sit down as soon as possible and let someone else call an ambulance, or call an ambulance yourself.
Diagnosis of diabetes
Which doctor should I contact if I suspect diabetes?
examine
There are no specific signs of diabetes that can be detected during the exam.
laboratory research methods
Instrumental Research Methods
diabetes treatment
Monitor blood sugar levels

diabetes diet
carb counting
The average carbohydrate content in the diet of people with type I diabetes should not exceed 17 units of bread per day.
- Limit caloric intake in all overweight patients;
- Minimize the amount of fat (mainly of animal origin) and sugar in food;
- Consume carbohydrates primarily from vegetables, whole grains, and dairy products;
- Eliminate or limit the consumption of alcoholic beverages (no more than 1 regular unit per day for women and 2 regular units per day for men).
Diabetes prediction and prevention
- engage in regular physical activity;
- A varied diet containing adequate fiber, protein, fat, and carbohydrates;
- healthy weight control;
- reduce alcohol consumption;
- Quit drinking and smoking.
Nutrition to prevent type 2 diabetes
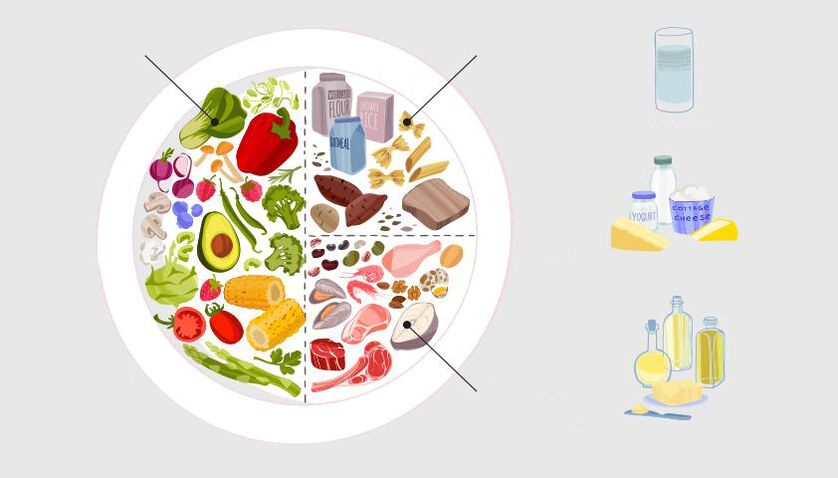
- drink when you are thirsty;
- Eat less salt, no more than one teaspoon (5-6 grams) per day;
- Limit the consumption of trans fats (found in many prepared and processed fast food products, cakes and pastries);
- Reduce consumption of saturated fat (found in sweet pastries, fatty meats, sausages, butter and lard);
- Eat less sugar, no more than 7 teaspoons (30 grams) per day.
























